Brief

Executive Summary
- Increasing National Health Service (NHS) productivity and turning around the past few years of deteriorating performance requires a multifaceted approach that targets the four management pillars of healthcare delivery: quality, operations, resource use, and finances.
- Successful transformations in performance and productivity require investment across all four management pillars simultaneously.
- Recent public scrutiny of the NHS’s financial problems, long waits, safety concerns, and declining user satisfaction opens the door for a transformational pivot. NHS leaders should capitalise on this opportunity to enact positive change and reclaim their status as trusted and internationally respected providers of universal healthcare.
- Local NHS leadership teams should prioritise wins in achievable micro-battles, then amplify those successes on a broader scale.
When UK Health Secretary Wes Streeting described the NHS as “broken,” just after taking office in July, newly elected British Prime Minister Keir Starmer embraced and reiterated the point.
During his first news conference as Prime Minister, Starmer said this of the NHS: “Everybody who uses it and works in it knows that it is broken, and we’re not going to operate under a pretense . . . that doesn’t express the problem as it is, because otherwise we won’t be able to fix the problem as quickly as we need to.”
Streeting and Starmer’s bold statements represent a much-needed moment of honest assessment, echoing years of mainstream reporting that uncovered troubling evidence of flat or declining productivity at the NHS since the Covid-19 pandemic.
Specifically, despite increasing its full-time employee staff by more than 20% between 2019 and 2024—a surge of some 250,000 whole-time equivalents—the number of appointments and procedures currently completed at the NHS has seen a small increase of approximately 5% when compared to equivalent data before the pandemic.
Calling attention to the NHS’s current underperformance does not undermine the intrinsic value of universal healthcare, which provides most services free at the point of access. Rather, it represents a call to action—a nationwide opportunity—to improve the health and well-being of everyone who uses and works in the NHS by transforming its operational productivity and delivering better value for money.
The current state of NHS productivity
In May 2024, an NHS England report revealed that its productivity had declined by 11% since the pandemic. Average wait times for hospital procedures have increased from 8 to 15 weeks, and there are now 7.7 million incidents of people on the waiting list to receive NHS care.
In addition to difficulties with treating illness, the UK is falling behind at preventing sickness. Since 2020, there has been a reversal in the centuries-long trend of increasing life expectancy. Moreover, deepening health inequities have emerged across the country between the wealthiest and the poorest and between those who are socially advantaged and those who are not.
These challenges have directly affected systemwide healthcare approval ratings: An August 2024 poll found that just 28% of UK respondents felt satisfied with the quality of services provided by the NHS—a record low.
In July 2024, the UK’s National Audit Office pointed to the NHS’s flailing productivity as a leading factor behind its dire financials, reporting that the system was facing a deeper than anticipated deficit of 1.4 billion pounds, with many insiders believing it could easily double that figure by the end of the 2024–25 financial year.
Given this challenging backdrop, the nagging question remains: What can be done to help pull the NHS out of its productivity and performance slump?
Delivering transformation through the four pillars of healthcare management
Improving NHS productivity won’t stem from a single, simple solution. Rather, the answer lies in a multipronged approach. Returning the NHS to pre-pandemic levels of productivity and efficiency—then charting a path to exceed those levels—will require steps to optimise patients’ experience, target long-term talent engagement and retention, and engage existing and future infrastructure effectively.
Systemic operational change requires a framework that builds on the balanced scorecard concept first outlined by Robert S. Kaplan and David P. Norton in the early 1990s. Building on this tried and tested approach, Bain has developed a management methodology to measure an organisation’s productivity and overall operational strength via its performance on four key pillars.
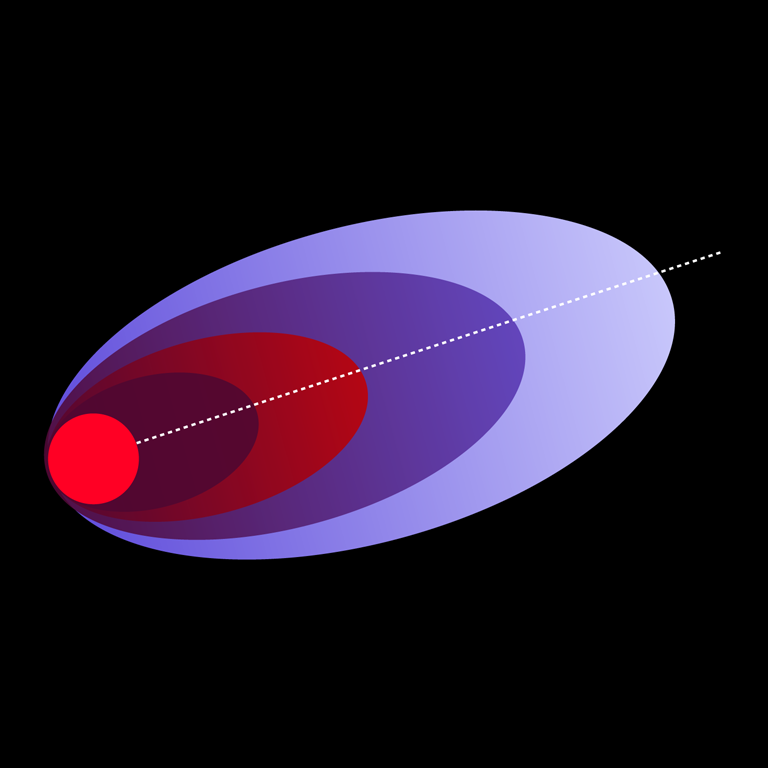
As shown in Figure 1, in the case of the NHS, those pillars are:
- Quality. Developed in the many clinical advances and reviews of the past few decades (and used by the Care Quality Commission), this includes safety and effectiveness, positive patient and staff experience, and an eye towards innovation and continuing professional development.
- Operations. Convenient, equitable, and timely pathways to care with rapid access to consultations, diagnostics, and treatments for planned and emergency services to increase overall activity and minimise wait times.
- Resource use. Productive use of people’s time, talent, and energy; maximising value from purchased goods and services; effective utilisation and maintenance of assets and infrastructure; reducing wastage and unsustainable consumption.
- Financial revenues and performance. Coding and billing effectively; strategic use of ancillary income and academic and shared services revenues; analysing and optimising income and expenditure margins for services provided to break even and invest in the future.
In the past, NHS leadership has, too often, selected a single pillar for financial investment and management focus while broadly ignoring the others. Such an approach is doomed to fail, as can be seen in the way the NHS has lurched between quality, access, safety, and financial short-term political and operational “imperatives” over the past two decades.
Similarly, robbing the future to pay for today—for example, by diverting capital investment away from critical infrastructure, digital modernisation, and professional development to cover the increasingly inefficient running costs of failing services—is a short-sighted and ineffective stopgap.
The typical NHS Cost Improvement Programme (CIP) offers a perfect example of such futile tactics. In an effort to reduce an identified deficit within a few months of the public sector’s fiscal year close, management attempts a mix of financial “grip and control.” Compounding the problem, leaders inevitably try to identify as many CIPs as possible, but since the lifespan of these cost-cutting schemes is, by definition, never more than a few months long, they rarely deliver transformative change.
In reality, successful investment and management focused on one pillar does not exist without forward-thinking investment across the board. Each pillar works in tandem with the others, and the success or failure of any single pillar affects the others accordingly.
There’s a flywheel effect at play here. As quality and efficiency rise, hospitals, general practitioners (GPs), and community care providers achieve greater care compliance among their patients and fewer follow-up visits and readmissions. This can lead, for example, to cost savings and improved margins, which can then be invested in innovation and professional development that further drive improvements to access and quality, and so on.
Prioritising management focus and gains in a particular pillar over the short term is permissible, but only if it doesn’t come at the cost of ignoring its impact on the other three pillars. Even when one pillar requires focus and attention, the other three pillars must also receive adequate attention or the law of unintended consequences will bite back.
Too often, CIP schemes force hospital management to focus on cash and balance sheet fixes rather than on sources of increased, recurrent value across the four pillars. As a result, their next fiscal year begins in no better position than the last, and systemwide quality, operations, and resource-use efficiency stagnate or, in the worst scenarios, deteriorate, sending the flywheel into full-throttle reverse.
To develop a path to successfully overcome its current performance and productivity challenges, the NHS should embrace positive change within all four pillars equally, working to ensure that a commitment to continuous improvement and adoption of innovation, technology, and best practices is shared by staff at every level.
A scalable approach to NHS transformation
Perhaps more than at any other time, there is now a sense of eagerness and urgency among NHS leadership, the UK government, and the general public to fix what’s “broken” with the NHS.
NHS leaders should capitalise on this momentum for positive change while being realistic about the scope of the job ahead.
Healthcare productivity is an amalgamation of multiple factors, each of which must be addressed if the NHS is to return to or, better yet, improve upon pre-pandemic productivity levels. These factors include:
- Workforce shape and size. The NHS must leverage its highly talented and multidisciplinary workforce to achieve much higher levels of targeted, effective results—not just activity for the sake of activity. Leadership should work to decrease employee churn, improve levels of staff engagement, and optimise skill and time management for its substantive workforce before calling on over-time and temporary staffing, as seen in our 2024 Front Line of Healthcare Survey.
- Clinical productivity. The NHS should target quality improvements that will deliver lower readmission rates for acute patient beds and other forms of failure demand and reduce waiting lists for elective procedures via virtual pre-assessment clinics, patient-initiated follow-ups, and better two-way digital communication, such as the NHS app, which lets patients conveniently administer their care pathways.
- Support function and procurement performance. Providers can increase their efficiency and financial stability by buying better, spending better, and reducing administrative complexity.
- Relationships between GPs, diagnostics, hospitals, community, and social care. NHS leadership should adopt a forward-focused approach to the site and type of care delivery that incorporates advice and guidance from appropriate secondary care specialists. Systems should also plan for care before referral and admission while prioritising the best fit for fastest access to services, patient choice, and convenience.
- Wider integration opportunities. The NHS can use scale to drive efficiencies while fostering cross-provider collaboration with primary and social care providers.
- Automation and generative AI technologies. Even though this appears as the final point in this list, it is not an optional add-on. Transformational wins will require new technology adoption in all the above points to secure incremental gains and more radical change.
The time for action is now
Bain’s Accelerated Performance Transformation (APT) adopts the four-pillar management approach to successfully help clients across a range of industries—including healthcare—build on existing strengths and identify attainable front line-led change initiatives supported by a Results Delivery Office to improve their performance and productivity.
This agile method of change management centres on:
- rapid, integrated diligence focused on finding high-value transformation opportunities using data analytics and professionally driven insights;
- accelerated value capture with a low burden of proof to drive and scale change quickly; and
- change that sticks by building the “muscle memory” of how change works within the organisation.
For NHS providers and systems, the most high-value, immediate transformation opportunities include addressing workforce pressures and balancing finances to forestall further debt.
The NHS should take immediate steps to secure safe and productive levels of staffing to meet current care delivery demands. At the same time, it must manage this workforce effectively, implementing efficient rostering and scheduling (underpinned by automated systems to match supply and demand and manage risk) to reduce wasted time and effort wherever possible.
To further secure its financial footing, leaders can tighten their approach to budget management and resource allocation across the board. This is often supported by steps to identify more cost-effective alternatives for essential services, reduce unnecessary operational expenses, or negotiate better terms with suppliers and vendors.
Transformational change at the NHS will be driven by hundreds of small changes rather than a single, large-scale “silver bullet” solution. But these small changes can save millions or even billions of pounds, particularly when scaled across trusts or across the entire system. For example, it’s possible that hospitals in just one city can save an estimated 80,000 pounds simply by standardising how they buy custard. They can cut costs by 40,000 pounds merely by curbing the automatic reordering of a single category of cardiology goods that are no longer essential.
While each example seems small, and even comical on its own, the compound effect of a leadership team that encourages and rewards its people to hunt out and deliver these opportunities can be the difference between being an organisation that is on course to achieve its full potential and in control of its own destiny and one that is in a spiral of financial decline, constantly dealing with time-consuming and energy-sapping regulatory intervention and scrutiny.
Winning through micro-battles
Accelerating the transformation of performance and productivity within a system as expansive as the NHS requires a scaled and distributed leadership and management approach. Leaders must first set for themselves then delegate for their service managers attainable key performance indicators that are balanced across the four management pillars.
In this way, they can achieve wins with small-scale, targeted initiatives—so-called micro-battles (see Figure 2). From those small successes, local leadership can encourage a “fail fast, win faster” culture, recognise and reward the wins as they come, capture best practices, and empower their own people with the task of dissemination and standardisation of the successful wins within larger operational scales or to other sectors.
The Micro-battles System® leverages the power of small targets driven by front line engagement that involve one or two enthusiastic drivers of change, such as an executive sponsor, divisional director, team leader, or front line clinician. Once these micro-battles have been achieved, leaders can build momentum within departments, wards, or specialties—or even between trusts—to scale the effect.
Executive, board, and system leadership’s key role within this strategy is to foster and amplify the positive effect of small-scale wins. In other words: Do it, prove it, disseminate it.
Many of the steps described above for transforming healthcare performance and productivity are tasks that NHS leadership could begin to implement right away. They demand no comprehensive legislative or policy changes or top-down reorganisation. Instead, they require commitment to a leadership and management approach that improves performance across all four pillars of quality, operations, resource use, and finance.
Accelerated Performance Transformation
One way to help mobilise the talent and energy of the front line and accelerate these leadership and management changes is through a long-term partnership with Bain’s APT programme. By signing up to be part of a Bain APT programme and adopting a relentless optimism in the innate capabilities of their staff and their mission to improve the health and well-being of the people they serve, NHS leaders and their teams can reap the full benefits that come from the energy, management expertise, and results-driven disciplines of a Bain team. In so doing, they can help turn the current public scrutiny of the NHS’s productivity and performance into an opportunity to reframe and re-earn the NHS’s status as an internationally respected provider of excellent value and universal healthcare. By taking this approach, these leaders will also be best placed to gain from reforms and investments the government makes in the coming months and years.

